Last updated on
Meet Our First Titan of Thrombosis: Professor Henri Bounameaux
We’re pleased to launch Titans of Thrombosis, a new series dedicated to honoring experts in the thrombosis field and showcasing their important contributions.

Professor Henri Bounameauxwas born in Belgium and spent most of his childhood in the Belgian Congo. He finished secondary school in Basel, Switzerland and received his medical degree from the University of Basel in 1978. After completing his medical training in Switzerland and Belgium, he returned to the University of Geneva in 1985 and has since served in several roles. In 1992, he founded the Division of Angiology and Hemostasis at the University. He was the Chairman of the Department of Medicine from 2002-2010 and has been the Dean of the Faculty of Medicine since 2011. After more than 40 years of dedicated work in the venous thromboembolism (VTE) field, Professor Bounameaux retired this summer. We had the privilege of chatting with him about his fruitful and far-reaching career.
Q: You’ve had an incredible career in the thrombosis field. What originally drew you to this area of study?
My father was a clinician-scientist and was interested in blood platelets. In my studies in Basel, I became interested in thrombosis and how it manifested in arteries and veins. I ended up doing my thesis on the topic of hemostasis, so I’ve really been in the field since I was a medical student. After that, I continued to be interested in lab-focused matters related to thrombosis, such as thrombophilia and anticoagulation.
Q: What has been the most important development in the field over the years?
I’ve been involved in all aspects of VTE and have witnessed a lot of changes over the past four decades! First, deep vein thrombosis (DVT) and pulmonary embolism (PE) are, in fact, the same disease, but they were managed by different departments when I started in the field.
Cardiologists or pulmonologists handled PE and internal medicine providers managed DVT. Clinicians didn’t communicate outside of their respective units, even though they were all caring for the same disease. Luckily, VTE has since emerged as a “unified condition” and has become more multidisciplinary.
I’ve seen changes in prevention and diagnosis, too. Prevention started in the 1970s when small doses of heparin were used in surgical patients to prevent post- procedure blood clots. Prevention now extends beyond surgical patients to patients in the hospital, patients who are immobilized, or patients who are otherwise at risk of developing a clot. There are now more medications and indications to prevent clotting.
We also used to use invasive tests to diagnose DVT, like venography of the lower limbs where you had to inject contrast dye into veins and then get x-rays to see the clot inside the veins. Another potentially dangerous procedure called pulmonary angiography was used to diagnose PE. These techniques had high complication rates in some cases. Since then, new tests have been developed that allow for noninvasive diagnosis in 99% of cases. VTE is also diagnosed more frequently because today’s methods are more sensitive.
And finally, we’ve seen huge changes in treatment options. When I started in the field, the only available medications we had were heparin and vitamin K antagonists (like warfarin). Over the years, we’ve been able to use things like low-molecular-weight heparin, fondaparinux, and direct oral anticoagulants (DOACs). The DOACs are now beginning to replace older medications. They’re more user-friendly, have fewer complications, are easier to take, and don’t need routine monitoring.
The field has changed in all aspects and has moved in the right direction!
Q: How has general awareness of VTE changed? Is it more recognized now than it was in the past?
Yes, awareness of the disease has definitely increased in the population. Some important people in the world have had thrombosis. We’ve all probably heard anecdotes about people who have had VTE after a long flight—those stories make headlines in the newspapers. However, I think patients still know less about this disease than about heart attack or stroke. General awareness could be further improved.
I do think awareness has improved in the medical community with the development of the diagnostic tools and “friendlier” treatments that I mentioned. The US Surgeon General’s Call to Action in 2008 also contributed to this awareness.
Q: What should a patient know after a VTE event? What’s an important take-home message?
Patients need to know that having one VTE event is the biggest risk factor for having a second event. So, if you’ve had the one, the risk of having a second one increases a lot. There are some “triggering” risk factors, like surgery or cancer, but VTE can recur in patients even without these “triggers.” Patients should recognize that VTE is a chronic condition, too. In fact, PE is the third leading cause of vascular death, so any patient who has had an event should receive treatment to reduce future risk.
Q: In your experience, what’s the best way to encourage patients to take their medication after an event?
This is an important issue that’s not specific to just VTE. For example, we know that only half of patients with high blood pressure will still be taking their medication 6 months after diagnosis. Treating VTE can be especially difficult because at the time of the event, patients usually take their medications. But 6 months later, some patients seem to have forgotten the event and stop taking their medications, which can be dangerous. Chronic disease is just that—it’s chronic— and many patients need lifelong treatment, whether or not they have symptoms.
I think that education is the only real solution to this issue. We need to repeatedly educate patients about VTE and what it means for them, and we need primary care providers to help us with this task. I guide my patients through the most active phase of their disease, but their primary care provider will follow them after that. Specialists and primary care providers need to work together to educate patients about how to take their medication properly and we must make sure that patients understand our instructions. We also need to have a discussion with patients about the risks and benefits of the medications.
One of the challenges we face with VTE medications is that the drugs can cause bleeding, so we need to balance the benefits and risks of the treatment. We need to check in with our patients and periodically reassess their medications because the risk of bleeding is something that can change over time. The role of the general practitioner cannot be overemphasized in all parts of this process.
Q: What do you think have been your most important contributions to this field? What are you most proud of?
First, I had a big goal when I began my career at the University Hospital [of Geneva]: I wanted to link the hemostasis lab with the clinical division of angiology. I envisioned a unified service that encompassed DVT and PE. I was exposed to this type of system during my fellowship and was impressed with what clinicians were able to accomplish when the lab and clinical unit were structurally linked. I was lucky enough to bring the model to my hospital in 1992. I just had to convince the authorities that this was a good idea—it took five years to make my idea a reality!
I think another major contribution linked to my name is the use of the D-dimer lab measurement in VTE/PE diagnosis. D-dimer is a protein fragment from the breakdown of a blood clot. If D-dimer isn’t present in a patient’s blood test, or if you find very low levels of it, you can rule out the disease. This was a big development in the late 1980s because it helped inform a non invasive diagnostic approach to VTE. In 1991, I published the first paper on using D-dimer as a diagnostic tool in The Lancet. Having a tool to easily rule out VTE was useful at that time and remains useful now. It helps us avoid irradiating and expensive diagnostic scans in patients.
Q: And now for the million-dollar question: what will you do in your retirement?

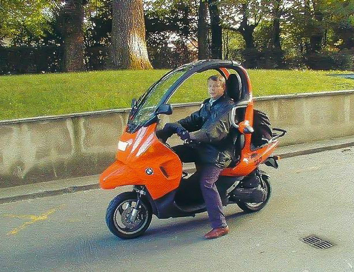
Well, most importantly, I’ll be working less! I’m going to concentrate on a few interesting things, the first being my family. I have six grandchildren and I’m very happy that I’ll get to spend more time with them. My wife and I enjoy horses as well. We actually have our own horses, so I’m looking forward to investing more time in this hobby. I’ll ride my motorcycle from time to time, too!
I’ll also stay involved in several intellectual activities. I’ll continue to serve as Chairman of the Board of the Academic Society of Geneva, which is a foundation that collects and allocates money for research at the University of Geneva. I will also maintain my position as the Vice President of the Swiss Academy of Medical Sciences. Finally, I’ll serve on the writing committee for the American College of Chest Physicians CHEST Guidelines for the Treatment of Venous Thromboembolism. I was a panelist on the last two iterations of these guidelines and am thrilled to contribute to the next edition. So, I think all of these things will keep me busy enough!