Last updated on
Patients Are Asking: Does Flying Increase My Risk for a Clot
Table of Contents
KEY POINTS
- When we travel far away from home, we may worry about getting a blood clot.
- The chance of getting a blood clot from traveling is small, but some have a higher risk, like those who are overweight, older, pregnant, have a history of blood clots, or have limited mobility.
- Airplanes have unique factors that can affect risk, like sitting in a tight seat and not being able to move around much.
- To lower the risk, try to move around every 1-2 hours, drink lots of water, and avoid sleeping or sitting in awkward positions for too long.
- Experts recommend these commonsense measures for most people, but those at higher risk may need to wear compression stockings or talk to their healthcare provider about taking medicine to prevent blood clots.
FULL SUMMARY

Home is where the heart is, though you might have to travel a long way to get there for the holidays. Long-distance travel may raise your stress level, but can it also raise your risk of getting a blood clot? Dr. Susan Kahn, a Professor of Medicine at McGill University and a Canada Research Chair in venous thromboembolism (VTE), weighs in.
Blood clots affect about 1-2 in 1,000 U.S. adults per year, and the risk may double or triple after a flight that’s 4+ hours. One study estimates that 1 in 4,600 travelers will have a blood clot within 4 weeks of a long flight. According to Dr. Kahn, “the actual risk of a travel-related blood clot is quite small, and the average traveler doesn’t need to worry about it. Billions of people travel by plane every year, and most of them don’t get a blood clot.”
However, those who already have risk factors for a clot may have a higher risk of developing travel-related VTE. These risk factors include:
- Obesity
- Age over 40
- Use of birth control pills or hormone therapy
- Recent injury or surgery
- Limited mobility
- Pregnancy
- A personal or family history of blood clots
- Active cancer or recent cancer treatment
It’s unclear if long-distance air travel is any riskier than car or train travel, but there are factors unique to airplanes that can affect risk:
- Air travelers sit in tight quarters with the back of the knee pressed against the seat. The vein behind the knee is a common area for clots to form.
- Immobility can raise the risk of a clot, but your seat assignment, turbulence, etc. can make it difficult to move around the plane.
- Your body takes in less oxygen when air pressure is lower, and some data suggest that lower oxygen levels can trigger the body’s clotting response.
- Dehydration may also increase the risk of a clot and drinking coffee or alcohol on a flight can fast-track dehydration.
- Many people sleep on flights – but if you’re sleeping, you aren’t moving or hydrating.
The good news is that there are several commonsense methods that can help lower your risk:
- Choose a bulkhead seat or see if your flight offers extra-legroom seating. If not, avoid putting a bag under the seat in front of you so you have more space for your legs and feet.
- Try to move around the plane every 1-2 hours. Selecting an aisle seat can make it easier to get up and walk.
- Avoid sleeping in awkward positions for long periods of time.
- Try not to cross your legs.
- Avoid wearing tight clothing.
- Drink lots of water and avoid alcohol, caffeine, and sedatives.
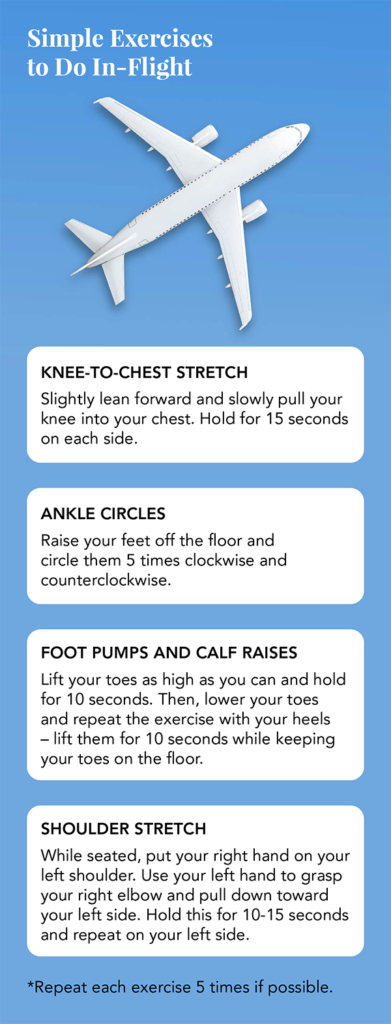
- Do some simple exercises in your seat to improve blood flow. (See picture at bottom.)
WHAT DO THE GUIDELINES SAY?
2012 American College of Chest Physicians (ACCP) Guidelines
Low-risk travelers should frequently move, perform calf exercises, and sit in an aisle seat if possible.
It’s suggested that high-risk travelers wear properly fitted, below-knee compression stockings while in flight.
Preventive blood thinners or aspirin are not recommended for long-distance travelers.
2018 American Society of Hematology (ASH) Guidelines
Compression stockings or anticoagulants/aspirin are not recommended for low-risk travelers.
“For the average healthy person taking a long flight, we don’t recommend anything other than commonsense measures, like walking around the plane and staying hydrated,” explains Dr. Kahn, who helped write the guideline.
ASH suggests that high-risk passengers use graduated compression stockings or a preventive dose of low-molecular-weight heparin (LMWH) for flights over 4 hours, If these measures aren’t practical, travelers can consider taking aspirin.
Because there’s still a limited amount of data on travel-related VTE, the ASH recommendations are conditional, meaning that the right course of action may be different for each patient.
The bottom line:
- Travel-related blood clots are rare.
- Moving around and staying hydrated are two ways to stay healthy – both in flight and on the ground.
- Travel-related VTE is an area that needs more research. Clear-cut evidence is lacking.
- Talk to your healthcare provider if you’re concerned about developing a blood clot while traveling.
References:
Blood Clots and Travel: What You Need to Know. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/dvt/travel.html. Updated February 1, 2019.
Kahn SR, et al. Chest. 2012;141(2):e195s-e226s.
Planes, Trains, and VTE. American Society of Hematology Clinical News. https://www. ashclinicalnews.org/features/feature-articles/planes-trains-vtes/. Updated March 1, 2019.
*Originally published in The Beat – December 2019. Read the full newsletter here.