Thrombosis is the formation of a blood clot, known as a thrombus, within a blood vessel. It prevents blood from flowing normally through the circulatory system.
Thrombosis can be deadly, and can affect any age, race, gender, and ethnicity.
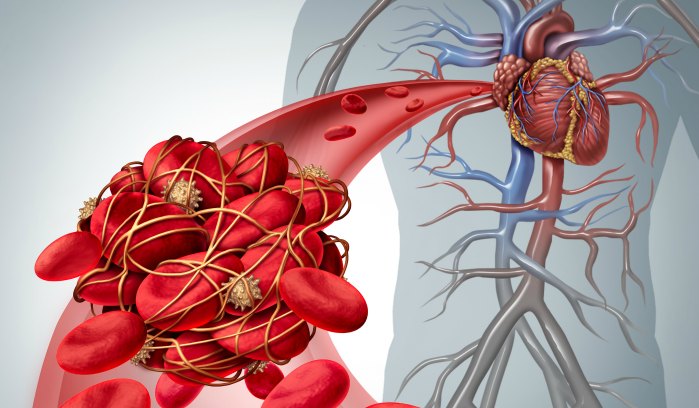
Blood clotting, also known as coagulation, is the body’s first line of defense against bleeding. When we hurt ourselves, our clotting system forms a “plug” or “seal” to protect us from losing too much blood. Our bodies often break down the clot after we’ve healed – but sometimes, clots form inappropriately or fail to dissolve after an injury. A blood clot that forms and stays in a blood vessel is called a thrombus.
Other medical terms used to describe blood clots include:
- Thrombosis: When a thrombus forms in a blood vessel
- Embolus or Embolism: A clot that detaches and travels through blood vessels to another part of the body
There are two main types of thrombosis:
- Arterial thrombosis refers to a blood clot that blocks an artery. Arteries carry blood away from the heart to other parts of the body. Arterial blood clots can block blood flow to the heart and brain, often resulting in a heart attack or stroke.
- Venous thrombosis, also known as venous thromboembolism or VTE, refers to a blood clot in a vein. Veins carry blood to the heart from other parts of the body. VTE is a condition that includes deep vein thrombosis (DVT) and pulmonary embolism (PE). Learn more about DVT and common symptoms. Learn more about PE and common symptoms.
Risk factors that contribute to thrombosis include:
- A hospital stay
- Surgery
- Major trauma, such as a car accident, fall, or head injury
- Infection
- Inflammatory or autoimmune disease
- Active cancer/chemotherapy
- Estrogen-containing birth control pills and hormone replacement therapies
- Pregnancy
- Obesity
- Leg paralysis
- History of heart attack or stroke
- Prior blood clot(s)
- Family history of blood clots
- Genetic or acquired clotting disorders
- Immobility (limited movement), including:
- Being on bedrest
- Being sedentary, meaning that you sit most of the day and are not physically active
- Traveling for long periods of time (4+ hours on a plane, car, or train)
Can blood clots be dissolved or removed?
The safest way to dissolve a clot is to let the body’s own clot-dissolving processes take effect. This can take anywhere from weeks to years, although some blood clots do not go away. In the case of massive or life-threatening clotting, clot dissolving drugs can be administered via catheter directly into the blocked blood vessels to dissolve recently formed clots. Thrombolytic drugs do come with a risk of bleeding. In certain emergency situations, clots can be removed surgically, but this increases the risk of further clotting.
What are the risks of blood clots recurring?
The chances of a recurrent blood clot is dependent on the circumstances leading up to the first clot. For example, if the blood clot occurred as a result of surgery or trauma, then the chances of re-occurrence is relatively low. On the other hand, for people who developed unprovoked blood clots and have stopped treatment after 6 months, the chance of recurrence is approximately 20% in the first 4 years and roughly 30% after 10 years.
What are the risks of taking an anticoagulant?
With all anticoagulant medications, there is an increased risk of bleeding. Signs of excessive bleeding can include prolonged nose bleeds, severe bruising, bleeding gums, vomiting or coughing up blood, and, for women, increased bleeding during menstruation. Patients with cancer, over the age of 65, and with renal or liver failure, face a higher risk of bleeding.
It is important for patients on anticoagulants to immediately seek medical attention if they experience:
- Head trauma
- A major accident, such as a car accident
- Unstoppable or prolonged bleeding
Patients who are concerned about risks associated with taking an anticoagulant should speak with their doctors about their concerns.
Recently Diagnosed?
Interested in learning more about diagnosis or joining a patient support group? Check out some of our resources!